PRE FINAL PRACTICAL EXAMINATION
A 70yr old male patient who has been a saree weaver by profession through his entire life with a proficient skill that comprised of manual labour started having complaints of
Intermittent urinary urgency and frequency with each void consisting of few drops of dribble from past 2 yrs, these episodes were very often with symptomatic relief in between, patient avoided to visit social gatherings in view of his symptoms, patient had intermittent burning micturition also for which antibiotics were given , was being followed up at a our hospital from one year. Patient underwent a cataract surgery 3 months back in view of progressive dimunition of vision which hampered his professional activity and limited him to household chores.
20 days back patient developed low grade fever with pain abdomen vomitings 3- 4 episodes in a day, diarhhooea 8-10 episodes/day large volume watery in consistency with no blood in stools for 1 week . In view of above symptoms patient was treated at a nearby hospital and went home when symptoms subsided.
From past 5 days patient is complaining of burning micturition with increased frequency and urgency.He also complains of reddish discolouration of urine. Patient’s wife informs that he has minimal oral intake of food and water from the past 10 days,and has also observed drastic loosening of clothes in the last one month.
Patient has no significant addictions with no significant family history.
There are no comobordities niether has the patient been on any previous pharmacotherapy
On General physical examination patient is conscious coherent well oriented to time place and person
He appears cachectic with features of dehydration such as sunken eyes dry tongue and loosened skin turgor.
Pallor & koilonychia present.
There is depletion of temporal pad of fat
Tongue is smooth with atrophy of papillae
Patient appears to be tachypneic
No raised JVP no pedal edema no anasarca.
Vitals at the time of admission:
BP = 90/60mmhg
PR = 90 bpm
SpO2 = 96% on RA
Temp = 98.0 F
Grbs = 60 mg/dl
SYSTEMIC EXAMINATION:
PER-ABDOMEN :
Inspection: patient has a scar of childhood branding.
All quadrants appear to move in symmetry.
No dilated & tortuous veins
No abdominal distension
No sinus tracts & discharging sinuses
Umbilicus is in normal position & inverted.
Palpation :
All the inspectory findings are confirmed.
Abdomen Soft & non tender.
Hepatomegaly present 2cms below the costal margin.
No splenomegaly.
Percussion:
Normal tympanitic note.
Auscultation:
Bowel sounds heard.
RESPIRATORY SYSTEM:
Bilateral supraclavicular &infraclavicular hollowing present.
Bilateral Air entry present
No added sounds.
CARDIOVASCULAR SYSTEM:
Apex beat localised to left 5th intercostal space 1cm medial to mid clavicular line.
S1 S2 heard. No murmurs, No thrills, no parasternal heave.
CENTRAL NERVOUS SYSTEM:
Higher mental functions - intact
Cranial nerves - Normal
Motor system - No abnormality detected
Sensory system- No abnormality detected
No signs of Cerebellar dysfunction.
INVESTIGATIONS :
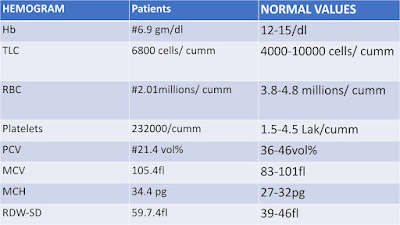
HEMOGRAM :
Urinary electrolytes:
Urine Na - 181
Urine K - 18
Urine Cl - 198
Chest xray-
Xray KUB
ECG
USG abdomen-
8mm renal calculus in left lower pole of kidney
Right moderate hydronephrosis
Left mild hyderonephrosis
PROVISIONAL DIAGNOSIS:
AKI(Intrinsic) ON CKD secondary to
? Partial HUS
? Secondary Adrenal insufficiency (Persistent hypotension and hypoglycemia in the hospital)
Anemia of chronic disease
Discussion-
Cause of Recurrent UTI in males- can it be attributable to h/o intermittent renal calculus
Patient has a wide gamma gap which can owe to chronic infections but in the back drop of anemia in this patient and systemic symptoms of fatigue weight loss - rationale to go for protein electrophoresis.
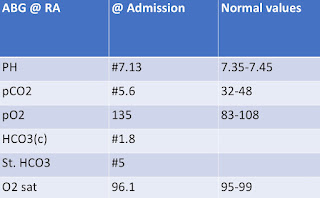
Should dialysis be done for an indication of refractory metabolic acidosis, although patient doesn’t have shruken kidneys with grade 1 RPD changes













Comments
Post a Comment